In the time it takes to read this sentence, someone, somewhere in America, will be in desperate need of blood. The American Red Cross estimates that the need arises every two seconds. When it does, it sets in motion a chain of events that are every bit as critical as the act of giving blood itself.
Donating blood makes heroes of ordinary people. Close to seven million people annually contribute to this vital cause, totaling over 13 million units of whole blood and red blood cells. One pint of blood can save as many as three lives.
With less than 38% of the population eligible to give, there’s a premium on blood products essential to treating a variety of conditions. Among the affected populations are cancer patients, hundreds of thousands of whom rely on blood transfusions as part of chemotherapy treatments; those who have sickle cell disease; and victims of trauma.
One car accident victim, for instance, may require up to 20 units of blood.
What is Blood Banking?
So what is blood banking? The American Society of Hematology defines it as “the process of collecting, separating and storing blood.”
The concept of harvesting human blood for medical experiments — first known as “bloodletting” — can be traced back thousands of years to the ancient Egyptians in 2500 BCE. Though as with most medical discoveries, the process has been drastically refined in recent centuries. Its crude origins have little in common with the modern practice.
Early attempts at human-to-human blood transfusions were, as one Chicago Tribune reporter put it, a “disaster.” But Austrian physician Karl Landsteiner was credited with a breakthrough in 1901 when he grouped blood into types A, B and O, paving the way for transfusion medicine.
World War II was the inflection point that ushered in the establishment of blood banks in the U.S. and abroad. First, in the 1930s, Soviet scientists recognized the need for blood to be preserved to retain its therapeutic properties, storing it in refrigerators and widely distributing it to local hospitals.
Then, inspired by the work of his Russian contemporaries, Chicago-based doctor Bernard Fantus established the United States’ first blood bank in 1937. Only it wasn’t yet known by that label; Fantus’ original choice — a blood preservation laboratory — was rejected for being too graphic. Fantus instead established the Cook County Blood Bank, and major urban centers such as San Francisco, Miami and New York followed suit.
The invention of the plastic bag in 1948 was another significant milestone in the modernization of blood banking. Until that point, impractical and cumbersome glass bottles were the preferred storage receptacle. But Boston-born doctor William Murphy recognized the advantages of storing blood in bags, which were much easier to transport and could be filled without exposing the contents to oxygen. It’s one of more than a dozen medical innovations credited to Murphy.
The FDA started regulating blood banking transfers in 1971, setting the stage for the oversight process by which blood banks are governed today. Facilities are frequently visited by inspectors who are responsible for assuring that high standards are met. The FDA works hand in hand with the U.S. Public Health Service to establish and enforce standards for the country’s blood supply.
What are Blood Banks?
As championed by the U.S. during World War II, the advent of transfusion medicine necessitated a central location for communities to store donated blood, screen it for infectious diseases, separate it into blood products, and catalog it for later use. Many of these facilities, known as blood banks, were constructed at existing hospitals, but others were conceived as standalone institutions. Today, the country’s network of blood banks accredited by the American Association of Blood Banks totals more than 2,400.
Blood banks require teams of skilled laboratory scientists to process samples efficiently and accurately. They do so in anonymity, under relatively calm circumstances — in stark contrast to their counterparts in bustling hospitals.
Yet, while the work of these specialists often goes unrecognized, it took on added significance amid the COVID-19 pandemic. With blood drives stymied by social distancing protocols, many blood banks endured shortages.
All the while, blood products remained in high demand, and so the medical lab scientists who prepare them set aside their own health concerns and continued to come to work. Blood banks and microbiology labs were refashioned as testing facilities for experimental plasma treatments, requiring lab workers to toil around the clock.
Explaining her motivation to the New York Times in December 2020, one lab technician remarked, “I do it because there is always more work to be done than the hours to do it in.”
That attitude reflects the gratification that comes with working in blood banks. These roles may not require direct interfacing with patients, but lab workers form meaningful connections, seeing the same names repeatedly and knowing they’re making a difference.
What is Blood Banking’s Role in Making the U.S. a Global Protector?
Soon after Bernard Fantus coined the phrase “blood bank,” the U.S. would begin to assert itself as a leader in global relief efforts, shipping plasma — a universal blood product — to Great Britain as the second Great War was raging. In 1941, the American Red Cross organized a civilian blood donor service to help millions of soldiers overseas, further solidifying the country’s devotion to the cause.
“Throughout our country’s history, the humanitarian spirit of the American people has shined as a beacon of hope in times of crisis,” President Joe Biden said in declaring March to be Red Cross Month in 2021. “It is written in our DNA that when hardship strikes, we come together to ensure that no one faces it alone. It is in that spirit that we celebrate American Red Cross Month, a chance to honor all those selfless Americans who step up and lend a hand whenever and wherever people are in need.”
Another American steward of the blood banking movement was Dr. Charles Richard Drew, who was a pioneer in more ways than one. As a Black man, he saw his groundbreaking work in transfusion medicine soured by racial discrimination; Black donors were not allowed to give blood in the U.S. until 1942, and it was done on a segregated basis until the early 1970s.
Drew, whose findings were pivotal to the innovation of storing blood in bulk, fought this injustice until he died in 1950. He once declared that the acceptance of Blacks in the various fields of medicine and physical science “has not only opened a small passageway to the outside world, but is carving a road in many untrod areas, along which later generations will find it more easy to travel.”
What Happens to the Blood We Donate?
Lab scientists stationed in blood banks meticulously guide over 100 samples per day through a journey of sorts, one that helps replenish the facility’s supply of in-demand blood products. Technology has streamlined this process over the years, but it’s still very much dependent on a small group of dedicated specialists whose attention to detail is crucial to the patients they serve.
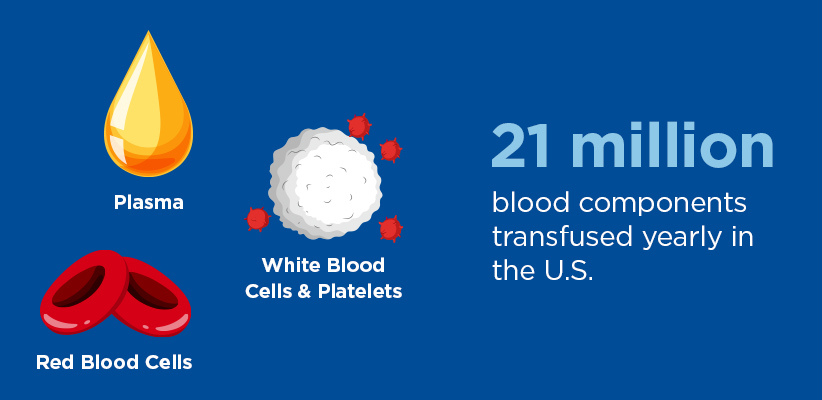
Upon arrival, the blood samples undergo a series of tests to ensure their safety and compatibility before getting spun and separated into red blood cells, platelets and plasma. Left untouched in a test tube for a period of time, the same products would eventually be visible: the red cells settle to the bottom; platelets, appearing as a white, fuzzy layer, would sit in the middle; and the pale yellow liquid known as plasma — which is water, proteins and electrolytes — floats to the top.
The red cell units are then organized by blood groups, with O-negative — known as “the universal donor” — being the most valuable commodity. Each is inscribed with an expiration date of 42 days from when they were collected and stored in refrigerators at four degrees Celsius.
Plasma units, which also have a limited shelf life, get frozen. They’re thawed on an as-needed basis in an automated plasma bath. Platelets are shelved on racks that look like something a bakery or kitchen might use, and a machine called an agitator keeps them constantly moving so they don’t clump.
Once a request comes in, a medical lab scientist locates the appropriate blood product and sends it to its desired location in the hospital. Emergency deliveries of blood come from the collection site or other hospitals and are delivered by courier or by taxi.
Donors on average give one component, or unit, of blood in one sitting, and that translates to about a pint. Nearly 21 million blood components are transfused in the U.S. each year, per the American Red Cross.
Transfusion are the most common application for donated blood. It’s used for traumatic injuries, burns, surgical procedures, infections, a variety of illnesses (including cancer, anemia and blood disorders) and blood loss after childbirth.
Most donors opt for giving whole blood donations, but they can also provide “power red” samples — which produce a concentrated dose of red cells — or choose to donate plasma or platelets specifically.
Donated blood also has non-clinical applications, such as developing and testing new treatment methods. Early on in the COVID-19 pandemic, for instance, the country invested hundreds of millions of dollars in researching plasma-based therapeutics before ultimately suspending the program.
Varied Paths to a Rewarding Career in Blood Banking
Medical lab scientists fill a variety of distinct roles within a blood bank. Generally speaking, each of these specialists possesses a certain skill set — an aptitude for problem-solving, dexterity with tools and lab equipment, computer proficiency and a keen eye for detail — and from there they occupy different posts along the timeline by which new blood samples become blood products.
Among the positions are regulatory experts, laboratory administrators, researchers, technical advisors, quality assessors and transfusion safety officers. In addition to private and public hospital blood banks, these jobs can be based at community blood centers, university-affiliated blood banks and independent laboratories.
The University of West Florida‘s online Medical Lab Technician to Medical Lab Scientist (MLT to MLS) bachelor’s degree program can help aspiring laboratory scientists who already possess an associate degree take the next step toward realizing their goals. It’s also specifically designed to help existing technicians further their careers by helping to equip them with the skills necessary to take on a supervisory role.
With an asynchronous, fully online format, students can work at the speed that suits their schedules as they navigate a diverse and rigorous curriculum. Among the topics taught by expert, field-experienced faculty are hematology, molecular diagnostics, diagnostic microbiology and physiology. Blood banks are a pillar of the country’s healthcare system, and the University of West Florida is preparing the next generation of compassionate laboratory scientists.
Learn more about the University of West Florida’s NAACLS-accredited online MLT to MLS bachelor’s program.

